Patient survey results show symptom and treatment histories of 124 respondents
In January 2005, we developed a questionnaire to document the treatment histories of many of the women who had written to us. Our goal was to combine individual responses and to report those trends on this survey page. Data was collected between January 2005 and June 2012, from 124 patients who reported pneumothoracies near the time of menstruation. Surveys from patients who reported symptoms but no verifiable lung collapses were not included. Surveys from patients reporting less than six months of treatment history were not integrated until at least six months of follow-up could be completed. Attempts to contact all patients for follow-up were made at regular intervals of approximately 12-18 months, and individual survey results were updated as patients provided new information. In many cases patient contact had been ongoing since 2005. It should be noted that all data presented here was obtained through patient self-reporting. We have no means of verifying the accuracy of the information provided by survey participants. The data is assumed to be correct as far as the patients themselves understand their conditions and their treatment histories.
Survey Results
Results are presented as the total number of responses for each answer, and in some cases as a percentage of the total number of respondents (124). Percentages are rounded to the nearest whole number.
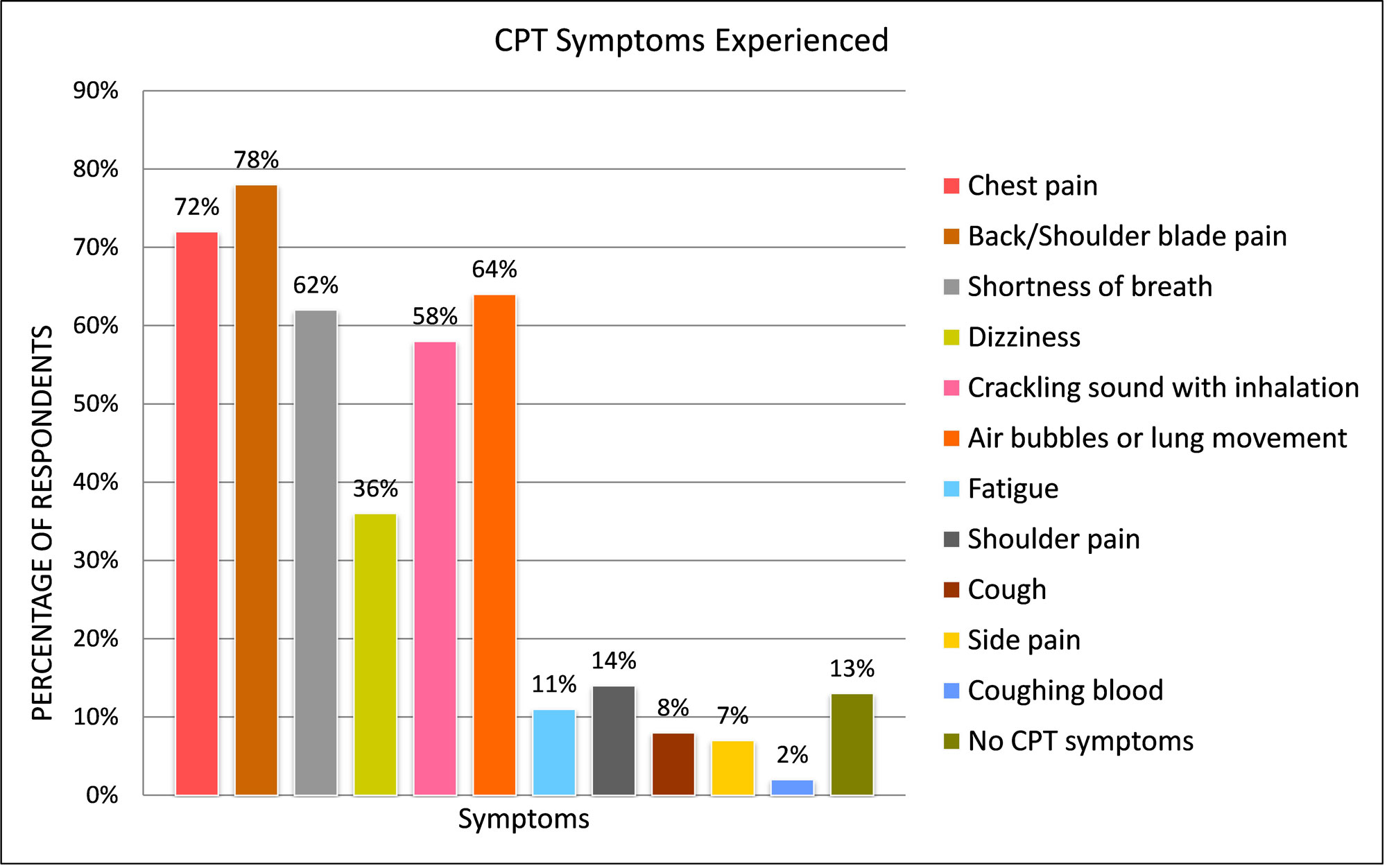
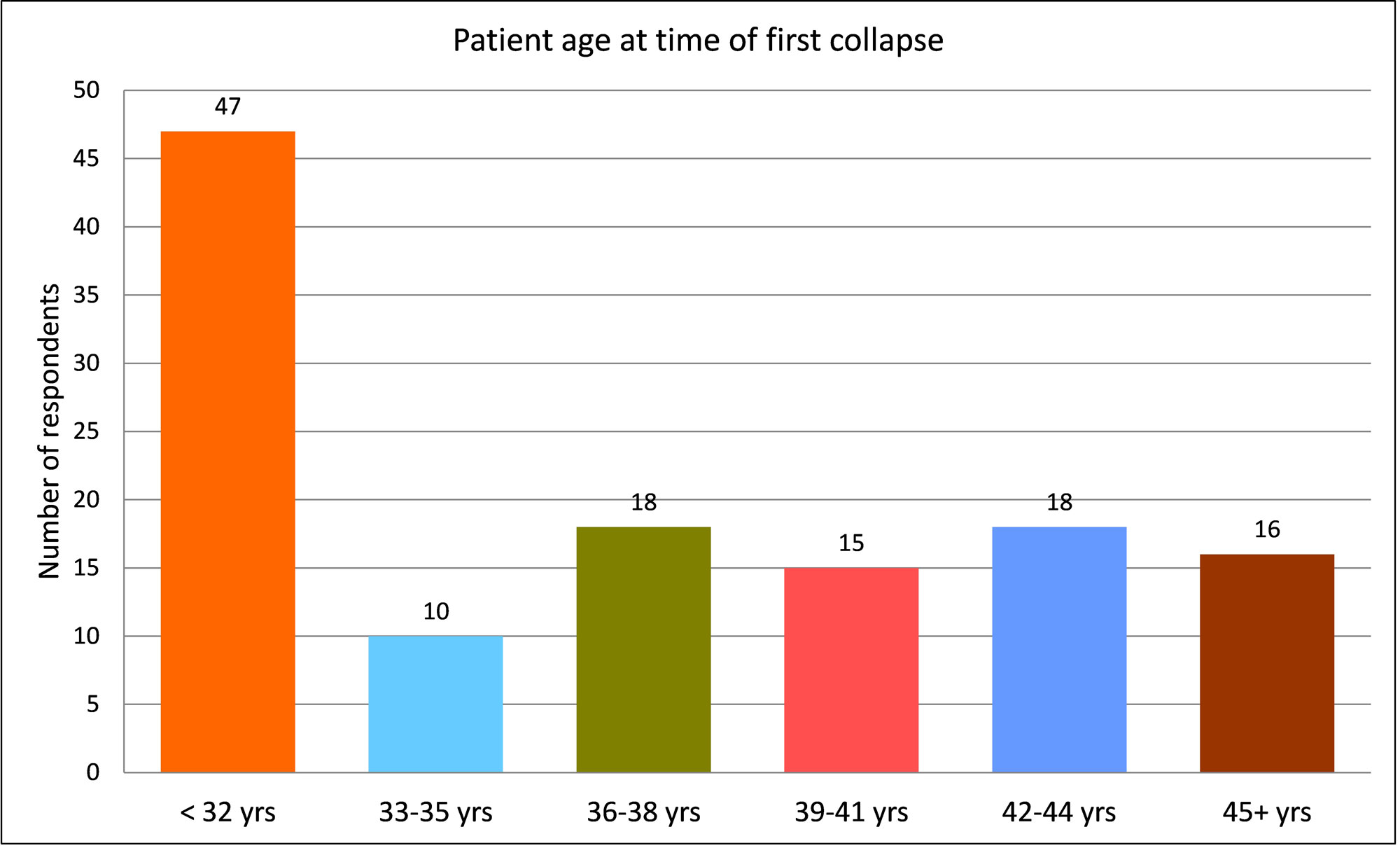
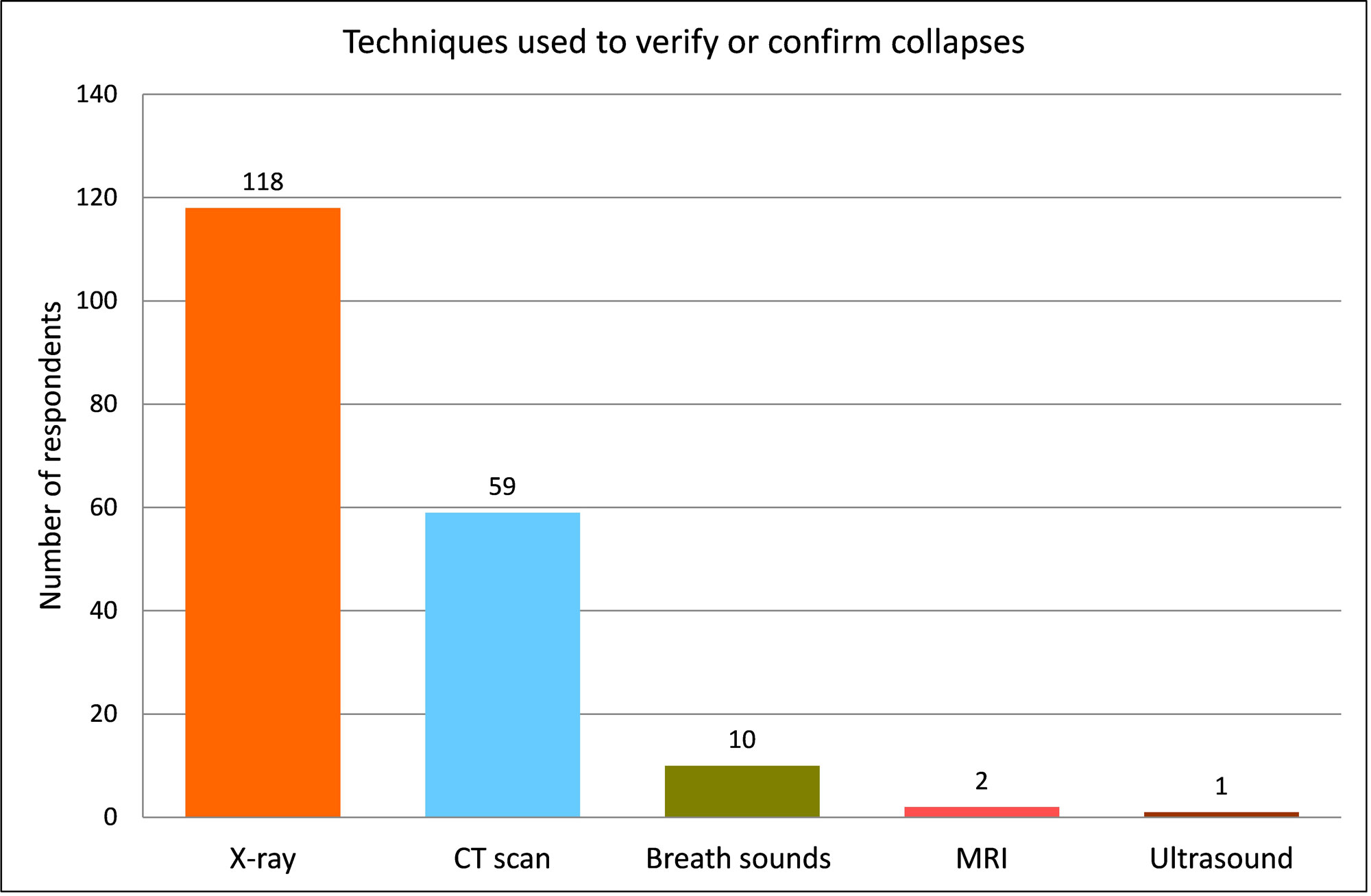
The first chart shows CPT symptoms by the percentage of women who reported having experienced them prior to or during their first collapse. Additional charts document patient age at the time of the first collapse, the involvement of one or both lungs, and the techniques used to verify or confirm collapses.
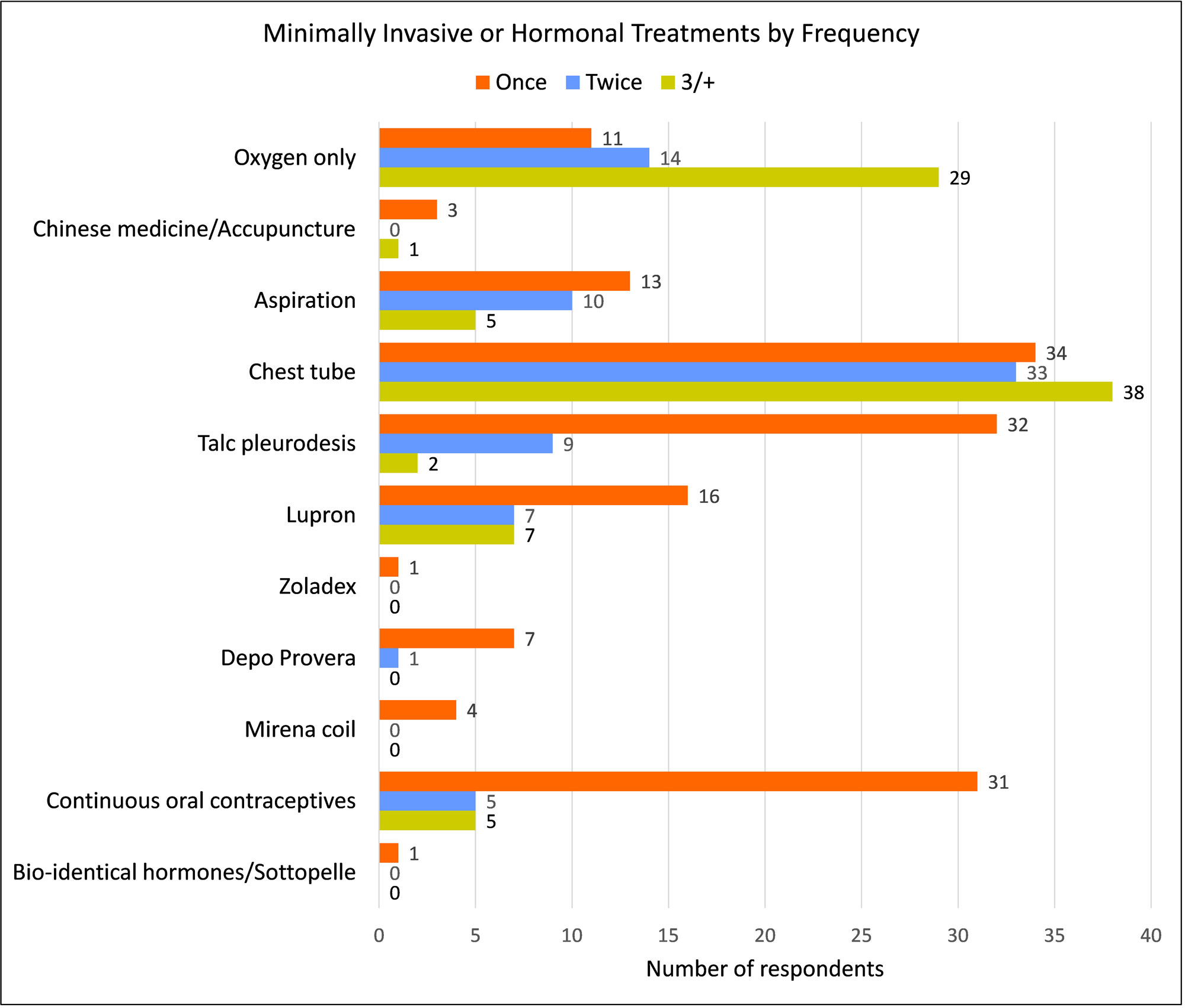
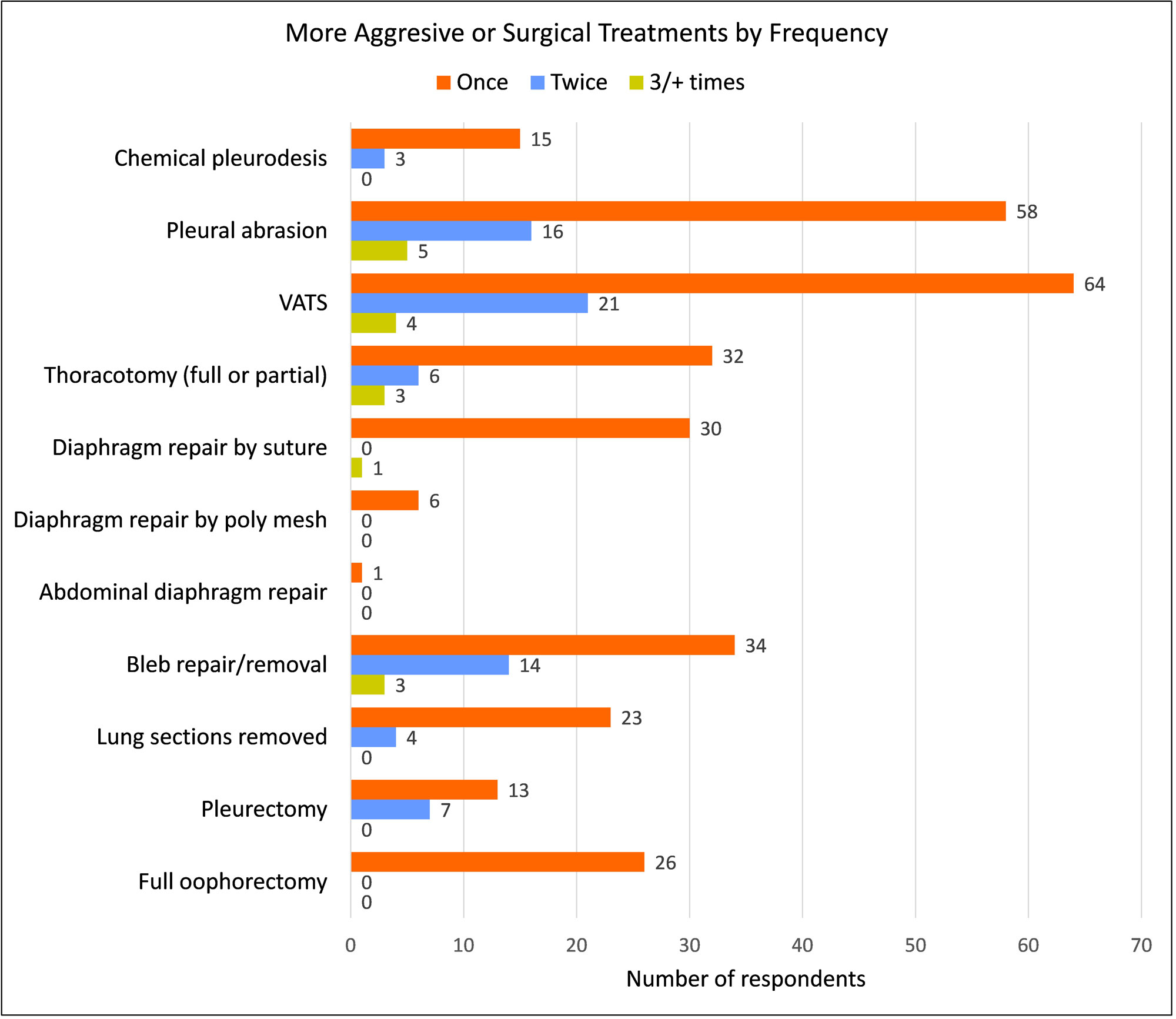
Treatment Frequency
Each treatment option shows the total number of women who reported having received it, detailed by the number of times they endured each one; once, twice, or three times or more.
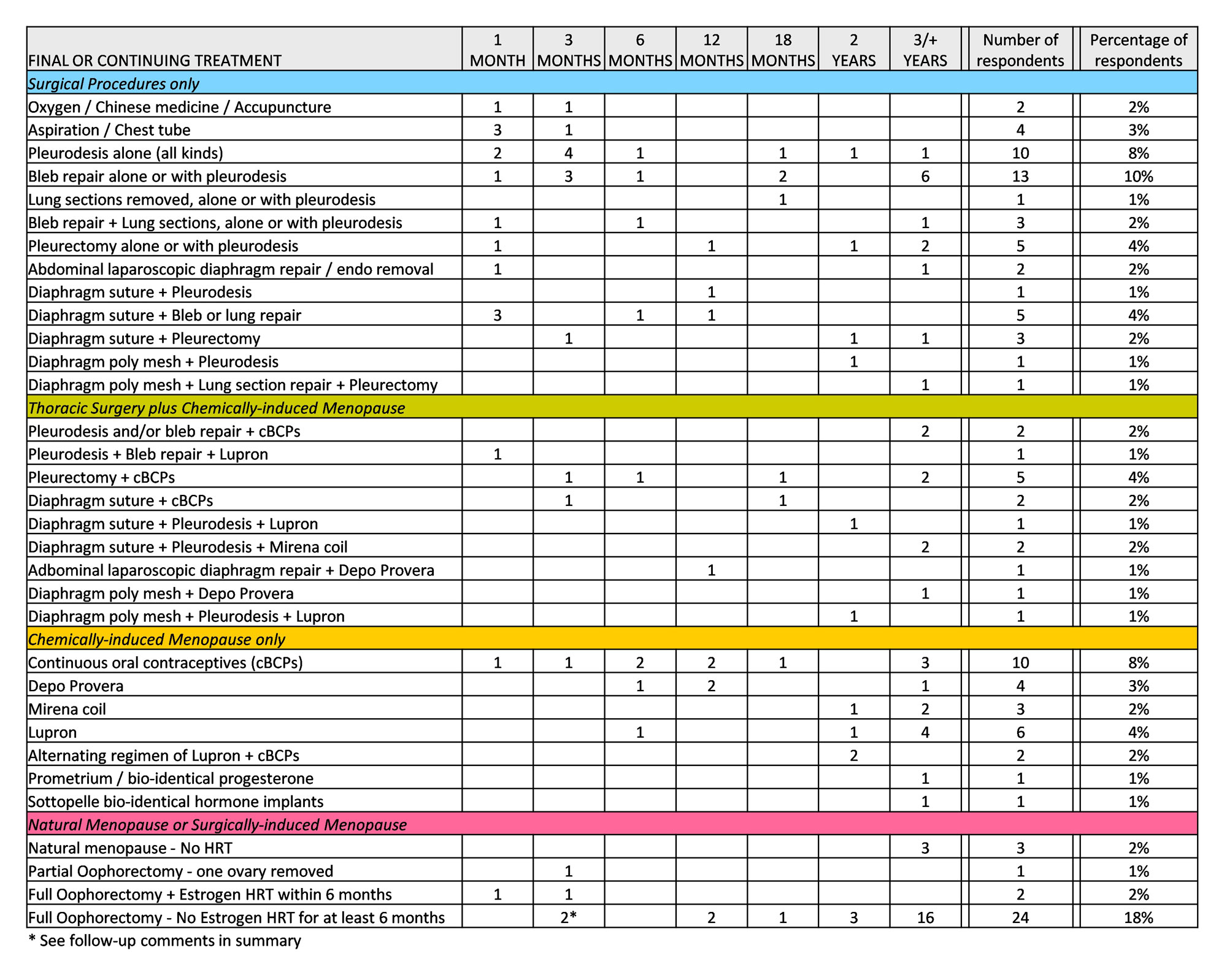
Length of Collapse-free Status Following Final/Last Treatment Received
Each treatment option shows the total number of women who indicated the treatment as their last by the number of months each has remained collapse-free. The final column displays an overall percentage of women who reported the treatment as their most recent. For this table, VATS and thoracotomy are understood to be the means by which the surgeon performs a repair procedure, but are not treatments in of themselves. In cases where multiple thoracic procedures were performed concurrently, or where hormonal treatment was administered immediately following thoracic surgery, they are so indicated. For clarity of display, treatments are divided into four basic categories: Surgical Procedures only; Thoracic Surgery plus Chemically-induced Menopause; Chemically-induced Menopause only; and Natural or Surgically-induced Menopause.
*For CPT patients* Please note that we are not physicians and are not providing medical advice. Results presented in this survey are reflective of the conditions of the ladies who have responded. We do not mean to imply that their treatment history will be the same for you. We present this data so that you can be better informed about treatment options, and able to discuss those options with your personal physician.
The most surprising result continues to be the reported age range for first-time collapses. 47 of 124 respondents (38%) indicated this age as less than 32 years old. While this trend was also reported in the 2011 update, the 2008 update reported this age as 39-41 years old, which is consistent with the age range cited in literature. With the vast amount of information online, it is reasonable that both patients and their doctors are now more familiar with the condition so that women are being diagnosed at an earlier age.
Survey results also indicate that treatments which include a plan to address the endometriosis are more successful than treatments which involve thoracic surgery alone.
42 of 124 women (34%) reported a collapse-free status of six months or less. Of these, 2 reported oxygen only or non-traditional treatment, 25 reported thoracic treatment alone as their most recent, 4 reported thoracic surgery combined with hormonal treatment, 1 reported a partial oophorectomy, and 10 were no longer menstruating due to surgical or chemical menopause.
82 of 124 women (66%) reported a collapse-free status of one year or more. Of these, 24 reported thoracic treatment alone as their most recent, 12 reported thoracic surgery combined with hormonal treatment, 2 reported bioidentical hormone therapy and 44 were no longer menstruating due to natural, surgical or chemical menopause. Of the 24 who reported thoracic treatment alone, 4 of them complained of continued monthly chest/back pain even though they remained collapse-free.
As mentioned above, 2 women reported the use of bioidentical hormone therapy in order to treat endometriosis by balancing the hormones. One reported using pharmacy compounded bioidentical progesterone. The second reported using Sottopelle bioidentical hormone implants. Both women reported a collapse-free status of at least three years, without pain even though they continued to menstruate.
25 of 124 women (20%) reported the use of synthetic hormones to stop menstruation (Lupron, Zoladex, Depo Provera, continuous oral contraceptives, etc). Of these, 19 reported a collapse-free status of one to three years.
30 of 124 women (24%) reported being in natural menopause or undergoing an oophorectomy (removal of one or both ovaries). Of these, 6 reported a collapse-free status of one to two years and 19 reported a collapse-free status of three years or more. 5 reported a collapse-free status of one to three months. Of those, 1 patient retained an ovary (and therefore continued to cycle), and 2 patients received estrogen hormone replacement therapy (HRT) immediately after surgery or within two months of post-op. The 2 remaining patients who reported continued collapses despite a full oophorectomy and no estrogen replacement were contacted for additional follow-up to clarify their situations. One patient indicated that her post-oophorectomy collapses were not following a cyclical or monthly pattern. She also said that these coincided with allergy season and occurred after episodes of heavy coughing or sneezing. This could suggest that perhaps strain placed upon a compromised diaphragm might be a problem, much in the same way that Lori experienced a small collapse during her laparoscopic nephrectomy after carbon dioxide gas distended her sutured diaphragm. The second patient reported that her symptoms and collapses were following a cyclical monthly pattern which suggests that she might still be cycling due to an ovarian remnant. In the 2011 update, we reported the case of another patient (now in the 3+ year category) who had also continued to suffer collapses after a full ophorectomy, until a second surgery found and removed, an ovarian remnant. Ovarian remnant syndrome is apparently not an uncommon complication after an oophorectomy. This example illustrates the importance of complete ovary removal for the purpose of treating CPT.
As can be surmised by the treatment choices of many women who have taken this survey, suppression of endometriosis by stopping the menstrual cycle remains a key point. Whether it be with Lupron or ovary removal, the goal seems to be estrogen suppression. Many doctors understand this goal in performing an oophorectomy, and encourage patients to wait at least 6 months before starting on any HRT. However, some obviously do not understand the dynamics of endometriosis and prescribe estrogen therapy immediately following surgery, thereby defeating the purpose of removing the ovaries in the first place.
Overall, surgical menopause still shows the best success rate in preventing collapses if both ovaries are removed and if HRT is initially withheld. All of the women who followed this treatment plan (minus the two outliers as explained above) remained collapse-free; most of them well over three years. However, it should be noted that surgical menopause while often successful, is not without its own problems. The most ideal treatment plan would address the endometriosis while leaving the menstrual cycle intact, as was the case with the 2 woman who used bioidentical hormone therapy. They were able to stop their collapses without the side effects of synthetic hormones or early menopause. Perhaps as doctors become more familiar with bioidentical hormone use, more women will be able to select this as a treatment option.
Additional survey results showed as expected, a trend of pelvic endometriosis and related menstrual problems. Most women experienced menstrual symptoms in their teens and 20's before being diagnosed with abnormalities in their late 20's or 30's. The menstrual symptoms most often reported were irregular cycle (50%), pelvic pain (52%), severe cramping (65%), and heavy flow (67%).
63 of 124 respondents (51%) had been diagnosed with endometriosis. Additional menstrual and pelvic conditions included uterine fibroids (19%), ovarian cysts (35%), infertility (22%) and anemia (22%).
Approximately 65% of respondents indicated the use of oral contraceptives, other progestins, or Lupron to treat menstrual problems.
For the women who were still having collapses, the most often reported future treatment plans under consideration included a full oophorectomy (14%), followed by the use of Lupron (8%).
We hope the results of this survey have been helpful to you as a patient and that the data presented here will encourage you to discuss all treatment options with your doctor.
To the many ladies who participated in this survey and have diligently responded over the years with your updates, a great big THANK YOU goes out to all of you! We could not have compiled this data without your help and are truly indebted to you for your steadfast support. Be encouraged to know that hundreds of other women will benefit, because you chose to share your stories with us. You girls rock! Thanks so much.